Reframing the objective
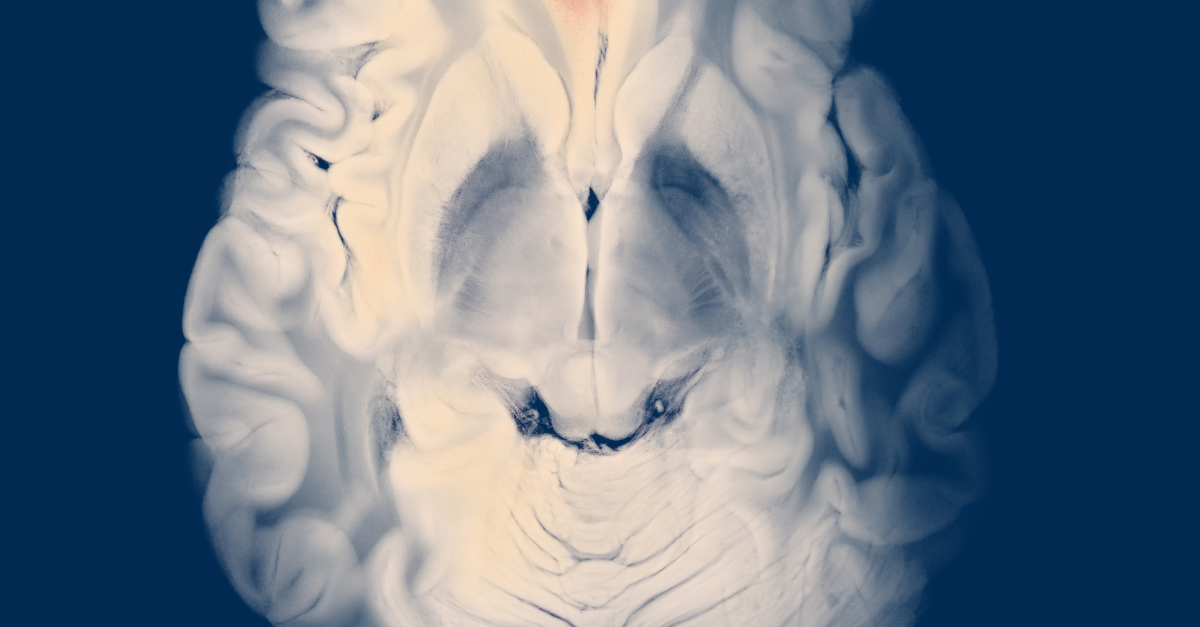
The nervous system learns slowly—through repetition, sleep, and a calmer internal environment. For many with neurological disorders, the winning strategy is not to outmuscle symptoms, but to quiet the background noise that keeps circuits unstable. By combining targeted cellular signaling with practical routines, programs in Panama aim to shift daily life from “unpredictable” to “steady,” meeting the brain where it is and teaching it to do more, more often.
Why mesenchymal signals matter
There’s a reason plans center on mesenchymal stem cells: they help temper neuroinflammatory cascades, provide trophic factors that protect vulnerable tissues, and support immune balance that prevents reactivity from swamping progress. In practice, this improves the “return on effort” from sleep hygiene, nutrition, and movement training—so improvements can accumulate instead of being erased by the next tough day.
The advantage of a destination model
Execution counts. The ecosystem supporting panama stem cells is designed to coordinate testing, infusion, education, and rehab inside one itinerary, reducing friction and preserving bandwidth for healing. That coherence also makes it easier for care teams to adjust cadence, dosing, or coaching based on real-time response rather than waiting weeks between scattered appointments.
From intake to action
Effective plans for neurological disorders stem cells begin with clear goals—fewer tremor-dominant hours, steadier gait for 20 minutes, or two-hour focus blocks without a next-day slump. Cadence and delivery routes are matched to those targets: systemic infusion to reset the global environment, plus targeted inputs and task-specific training for priority pathways. The arc is designed to build cumulative effect, not rely on a one-time bump.
What the focused week looks like
Day one aligns baselines and expectations; day two often starts systemic infusion; days three to five integrate skill practice to help the nervous system use the calmer state—posture and balance drills, dual-task exercises for cognitive–motor pairing, and breath-led sleep timing. Within neurological disorders stem cells panama, education is practical and brief by design, so the plan is realistic at home without special equipment.
Money is part of medicine
Adherence rises when finances are clear. Programs that prioritize affordable stem cell therapy present bundled inclusions and timelines up front, so families can plan not just the clinic days, but travel, recovery windows, and follow-up check-ins. Cost transparency reduces anxiety and supports the consistency that neurological recovery demands—steady inputs over time, not intensity in fits and starts.
The expected progression
Early wins include smoother transitions, better sleep continuity, and less sensory overwhelm. Weeks two through eight often bring steadier balance, fewer reactive dips, and improved endurance for daily tasks. By months three to six, many patients report that the good days outnumber the unpredictable ones; life planning feels safer, and activities that used to have a “next-day price” become routine again. The success metric is a baseline that supports living, not tiptoeing.
Aftercare that multiplies signals
Cellular input fades unless reinforced. The take-home plan is short and specific: light conditioning to support autonomic balance, mobility to maintain joint and postural alignment, protein-forward meals to stabilize energy and repair, and a consistent bedtime with morning light to lock in circadian rhythm. Tiny anchors—two minutes of breathwork, a balance hold while coffee brews—help progress survive normal life.
How to choose wisely
Look for clear measurement, explained mechanisms, and plans that adapt to response. Ask how home routines are taught and how follow-ups are scheduled to correct course. When the program aligns credible biology with integrated logistics and honest budgeting, advanced care stops being a leap of faith. It becomes an organized path—small steps, repeated, turning possibility into function that lasts.