Reframing the objective
Immune suppression can be necessary, but it is rarely sufficient on its own. The stronger objective is recalibration: lower the misdirected attack while supporting tissue repair and the daily behaviors that maintain stability. Programs tailored for autoimmune diseases are designed around that goal—mechanisms that make biology more cooperative, delivered inside a system that makes follow-through easier.
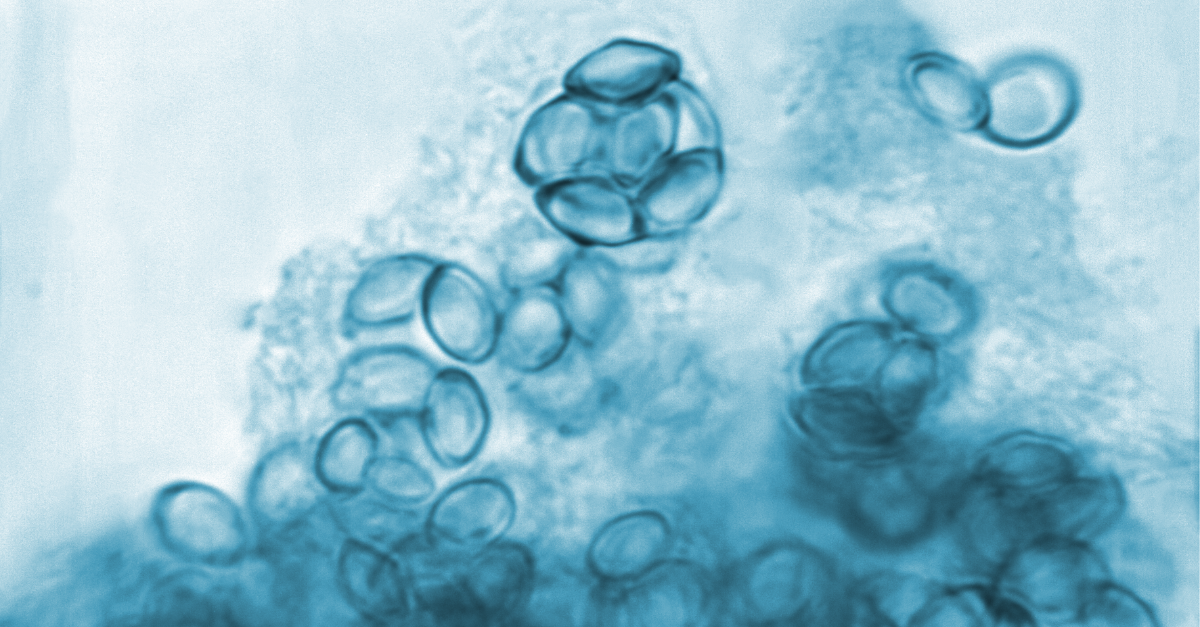
The role of mesenchymal signaling
Plans center on mesenchymal stem cells because they modulate inflammatory pathways and release growth cues that encourage reconstruction in joints, gut lining, skin, and more. As the background calms, patients see a better “return on effort” from nutrition, sleep, and movement—less fragility, fewer dramatic setbacks, and a trend toward steadier weeks.
Why delivery design matters
Execution turns a strong mechanism into lived results. In the ecosystem for panama stem cells, diagnostics, dosing, administration, and education occur under one coordinated itinerary. This coherence reduces cognitive load and helps ensure patients spend energy practicing the routines that make biological gains durable.
Program architecture that compounds
Effective protocols for autoimmune diseases stem cells begin with measurable goals that matter: fewer flare days, half the morning stiffness, a return to 30-minute walks or two-hour work blocks without a crash. Systemic infusion typically resets the inflammatory baseline; targeted support focuses on the most symptomatic tissues; and a written aftercare plan ensures the handoff from clinic to home is seamless.
A focused treatment window
Day one clarifies baselines and priorities; day two often begins infusion; subsequent days layer practical skills—breath for autonomic balance, mobility for range and posture, protein-forward meals to steady energy—so improvements survive normal life. The autoimmune diseases stem cells panama framework is intentionally simple: fewer obstacles, clearer steps, stronger adherence.
Budgeting that strengthens adherence
Financial clarity is clinical. Programs grounded in affordable stem cell therapy spell out inclusions and timelines—consults, labs, preparation, administration, and follow-ups—so families can plan travel and recovery without fear of surprise add-ons. Public guidance on stem cell therapy cost in Panama helps match program tiers to goals and resources, keeping the full arc achievable.
Context within destination medicine
Patients choose structured stem cell treatments in Panama because advanced protocols are paired with patient-first logistics that protect momentum. Safety, sterility, and education are built into a single plan, making it easier to implement at home. In practice, this reduces detours and increases the odds that incremental wins become the new baseline.
The six‑month pattern
Month one often brings calmer mornings and better sleep continuity; months two to three commonly yield fewer flares, steadier joints or gut rhythms, and a cut in “rescue” tactics; months four to six consolidate capacity—sustained workdays, social plans kept, walks or workouts without next-day penalties. The measure that matters is reliability: more good days, linked together.
The minimalist aftercare that endures
Short lists win. Twice-weekly strength stabilizes joints and metabolism; daily mobility preserves glide; low-impact conditioning supports endurance; protein- and fiber-forward meals reduce inflammatory noise; and a consistent sleep window locks in repair. With brief check-ins, the plan adapts to reality so improvements stack instead of slide.
Choosing with confidence
Ask how the protocol tracks progress, flexes cadence or dosing, and supports behavior change after departure. Confirm inclusions, timelines, and education, and how each connects to outcomes. With credible mechanisms, integrated delivery, and transparent planning, the path from flare to flow becomes practical—not theoretical—inside a patient-friendly model of care that puts stability within reach.