Neurological disorders touch almost every part of life: movement, memory, mood, speech, and independence. While conventional approaches can slow progression or manage symptoms, many families look for solutions that target the underlying biology—chronic neuroinflammation, disrupted immune signaling, and impaired repair. A structured, regenerative approach provides a way forward: reduce inflammatory noise, protect vulnerable tissue, and support functional recovery with a clear plan.
The neurological reality is complex. Conditions like Parkinson’s, Alzheimer’s, multiple sclerosis, ALS, traumatic brain injury, and stroke sequelae often present with overlapping challenges—fatigue, cognitive change, gait instability, tremor, sensory disruption. Effective care must be multi-layered and sustained. This is where high‑quality programs that incorporate neurological disorders protocols can make a meaningful difference by aligning cellular science with practical delivery and long‑term aftercare.
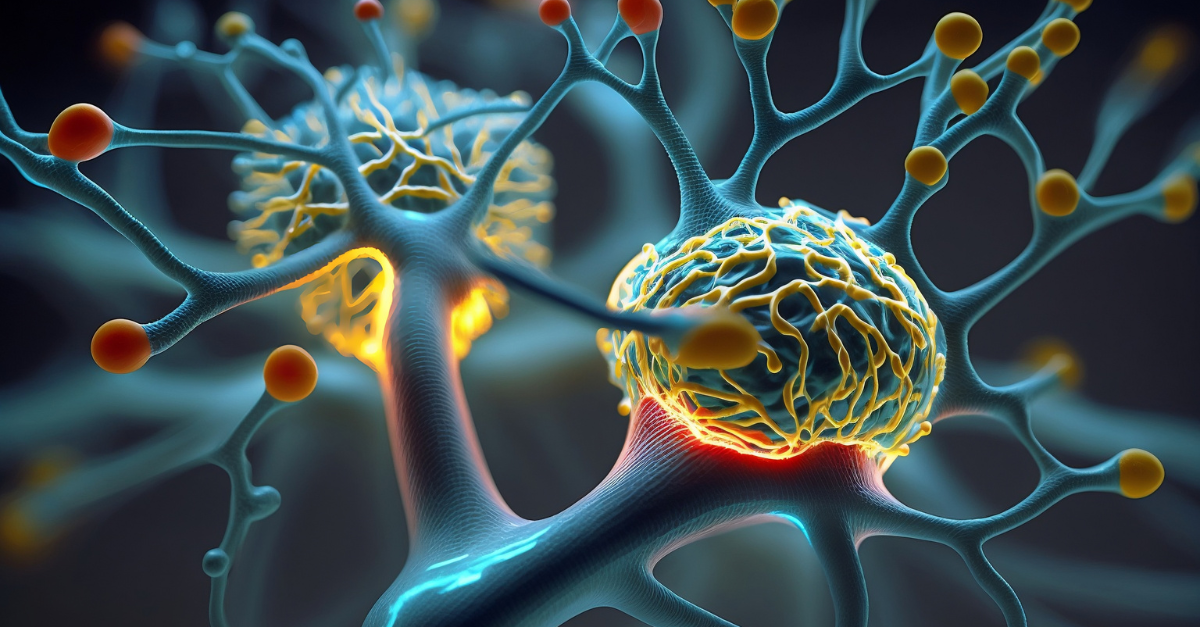
Why mesenchymal cells matter
At the heart of modern regenerative neurology are mesenchymal stem cells. These cells do not “replace” an entire neural network; instead, they create the conditions where repair is more likely. They modulate immune activity, reduce inflammatory signals, and release trophic factors that support neuronal and glial health. In practice, patients often report calmer nervous systems, steadier gait, improved endurance, clearer focus, and better sleep over time when these protocols are paired with rehab and lifestyle alignment.
A structured path to improvement
Programs tailored for neurological disorders stem cells begin with a comprehensive intake—history, diagnostics, and functional goals—so dose, delivery, and cadence are matched to the person rather than the label alone. Systemic administration can address widespread neuroinflammation, while targeted delivery may be considered for specific symptom clusters. Milestones guide follow‑ups, and adjustments are made as recovery unfolds.
Why Panama for regenerative neurology
A strong program requires not just science, but a setting that preserves energy for healing. The ecosystem supporting panama stem cells emphasizes organized schedules, clinical rigor, and a hospitality‑forward experience. When logistics are clear and aftercare is integrated, adherence improves and gains become more durable.
Affordability with transparency
A defining strength of this model is clarity around access. With a commitment to affordable stem cell therapy, programs typically outline bundled inclusions—from evaluation and lab work to cell preparation, administration, and structured follow‑up. This transparency helps families plan responsibly and track outcomes with confidence.
What meaningful progress looks like
Early improvements often include better sleep depth, calmer mornings, and smoother transitions in daily routines. Over weeks, gait mechanics, stamina, and attention span can improve; over months, those gains become baseline, with fewer “bad days” and more predictable capacity. Recovery is rarely linear—it’s a staircase. Tracking milestones at 6 and 12 weeks supports smart adjustments without derailment.
A whole‑journey mindset
Cellular therapy is a catalyst. The day‑to‑day work—rehabilitation, mobility, sleep, nutrient‑dense nutrition, and stress regulation—turns signals into function. This is why high‑performing programs build aftercare into the plan for neurological disorders stem cells panama: consistency makes improvements durable.
Getting started
A clear starting point is a candidacy review, three measurable goals for 90–180 days, and a written aftercare roadmap. With aligned expectations and a structured plan, families can build toward steadier, more capable days—one step at a time.